

Procedure Details
The patient presented with an old amalgam (silver) filling that had began to fall out over time. The tooth appeared to have some cracks and it was clearly visible that small pieces of the filling were missing. After performing an exam and xray, Dr. Patel diagnosed that the tooth was fractured and had current decay close to the nerve. Due to the failed existing restoration, extent of decay and condition of tooth structure, Dr. Patel recommended a build up, crown and pulp cap as treatment. The tooth was excavated, removing all present decay. During this process, laser treatment was used to access decay from under the gum line and remove the unhealthy gum tissue . Decay had reached close to the nerve, so a pulp cap was placed. A pulp cap is a material used to protect exposed nerve that is still healthy, in order to help prevent a root canal. The tooth was then built up to provide a proper base for the crown. Using the CEREC computer and milling chamber, Dr. Patel conveniently scanned the area, designed a crown and cemented it all in the same day. This eliminates the hassle of taking impressions and dealing with a temporary crown while waiting for a lab to finish the process. The patient's crown was cemented and proper adjustments were made for a correct fit and bite. He continued to return for his routine hygiene visits.


Procedure Details
The patient came in for an emergency, due to a broken crown on a front tooth. Her main concern was saving the tooth and having treatment completed the same day, as it was a cosmetic concern when she spoke or smiled. Visually, it was noted that the crown had broken and the metal post inside was exposed. The gum tissue surrounding the tooth had become diseased and overgrown, due to the presence of decay. Dr. Patel was able to determine that the decay had reached sub-gingival, meaning very deep, below the gum line and he recommended using laser gum treatment for access. This technology combines laser energy with a gentle stream of water which allows Dr. Patel to remove the diseased tissue, then access and remove all decay. The tooth was then prepared with a build up, post and new crown completing treatment the same day. The patient was given post operative instructions and will continue on their routine hygiene schedule in our office.


Procedure Details
The patient presented with a gap between her two upper and lower front teeth. During an exam, Dr. Patel was able to diagnose that the frenum (connective tissue) in both areas had began to pull, causing gum recession and diastemas (spaces between teeth). Not only did this cause a cosmetic concern for the patient, but there was also risk of periodontal disease due to the gum recession. Dr. Patel recommended a frenectomy of both areas and with the assistance of our Waterlase laser, the connective tissue was removed. After minimal healing time the patient was able to return for her routine hygiene visits.


Procedure Details
The patient presented with a history of periodontal disease. After a thorough exam and review of his digital x-rays taken in our office, Dr. Patel diagnosed that the patient had aggressive Periodontitis which had resulted in bleeding gums, bone loss, inflammation and some mobile teeth. Dr. Patel recommended that the patient undergo scaling and root planing to address the present plaque, calculus and stain on the surface and roots of his teeth. The patient was placed on a three month cleaning schedule and educated on the importance of maintaining good homecare. During these routine visits the patient's gum tissues were evaluated and continued to reveal deeper pocket depths around his teeth. Due to the continued poor prognosis of his mobile teeth and severe periodontal disease Dr. Patel recommended laser gum surgery. This allowed him access below the gum line to remove all bacteria, diseased gum tissue and decaying bone. The roots of his teeth were again scaled and smoothed and the bone was recontoured. Using the laser eliminated the need for scalpels and sutures which resulted in minimal bleeding and pain. This allowed faster healing, promoting healthy gum regrowth. We continue to monitor the patient's oral health and educate him on the importance of his homecare.


Procedure Details
This patient presented with chronic periodontitis which had resulted in inflamed bleeding gums, overgrowth of tissue and bone loss with deep pockets. Due to his poor homecare, being an active smoker and his aggressive periodontal disease, Dr. Patel recommended he undergo laser gum treatment. The patient however, requested to start with scaling & root planing first. The scaling & root planing was performed to address the present plaque and calculus on the surface and roots of his teeth. He was educated on the importance of good homecare and provided proper oral hygiene instructions. When the patient returned three months later for his periodontal maintenance, his hygiene had not improved and he was still an active smoker. Dr. Patel recommended proceeding with laser gum surgery. This allowed him access below the gum line to remove all bacteria, diseased tissue and decaying bone. The roots of his teeth were again scaled & smoothed and the bone was recontoured. Using the laser eliminated the need for scalpels & sutures, which resulted in minimal bleeding and pain. This allowed for faster healing, promoting healthy gum regrowth. Dr. Patel continues to monitor the patient's oral health and educate him on the importance of his homecare.


Procedure Details
The patient presented to us after having a wisdom tooth extracted at an oral surgeon's office. The tooth in front of the one she just had removed appeared to have a black spot on the side surface and the biting surface was worn. The gum tissue surrounding the tooth appeared inflamed and overgrown. Upon examination, there appeared to be a "flap" of tissue between the extraction site and existing tooth where a drainage of pus had developed and an x-ray confirmed that decay was present as well. Dr. Patel prescribed antibiotics and drained the infection site. The decay was cleaned out of the tooth and a composite "tooth-colored" filling was placed. The patient returned a few days later for laser treatment. Dr. Patel used our Waterlase laser to remove the overgrowth of tissue surrounding her tooth as well as all remaining infection inside and around the bone. The patient returned regularly for follow up appointments to monitor the area and was able to continue with her regular hygiene schedule in our office.


Procedure Details
The patient presented with inflammation and a loose implant abutment and crown, due to an overgrowth of gum tissue and Peri-Implantitis. The gum tissue had become so overgrown and inflamed that it had essentially "pushed" the abutment and crown out of the implant. Using the WaterLase laser, Dr. Patel removed the overgrown tissue and bacteria around the implant surface. He was able to decontaminate and re-contour the bone that was lost due to the peri-implantitis. Finishing the treatment process with the WaterLase, Dr. Patel disinfected the original abutment and crown, so the patient was able to utilize them once again.


Procedure Details
The patient presented in pain for an emergency appointment. A tooth on her upper left had become loose and an x-ray revealed a large infection. Upon examination, Dr. Patel diagnosed that the tooth was decayed, fractured and had become periodontally involved. The significant bone loss resulted in unrestorable mobility and required extraction. Once the tooth was removed, Dr. Patel used the laser for infectious tissue removal and bone disinfection. A bone graft was placed to support a replacement restoration and once the site had fully healed four months later, an implant was placed. The patient returned at a later date for the implant crown and she continued on a regular hygiene schedule that included implant maintenance.


Procedure Details
While in town visiting, the patient broke a tooth that had recently been filled back home. She was having pain and needed to be seen right away. The tooth was broken, fractured and endodontically involved, meaning there was decay into the nerve. Dr. Patel's diagnosis provided the patient with two different treatment options to either save the tooth with a root canal and crown, or extract it. She decided to save it. Dr. Patel excavated the tooth and removed all decay with the help of our Waterlase laser. The Waterlase was used to access decay below the gum line, as well as disinfect the area. Once the canals were cleaned out, they were filled with a material called "gutta percha" and then sealed off. A post was placed inside for stability and then the tooth structure was built up to support placement of a crown. Using our CEREC computer Dr. Patel took a digital scan of the tooth and a crown was made in our CEREC milling chamber the same day. Once cemented, any necessary adjustments were made to ensure a correct fit and bite.
Procedure Details
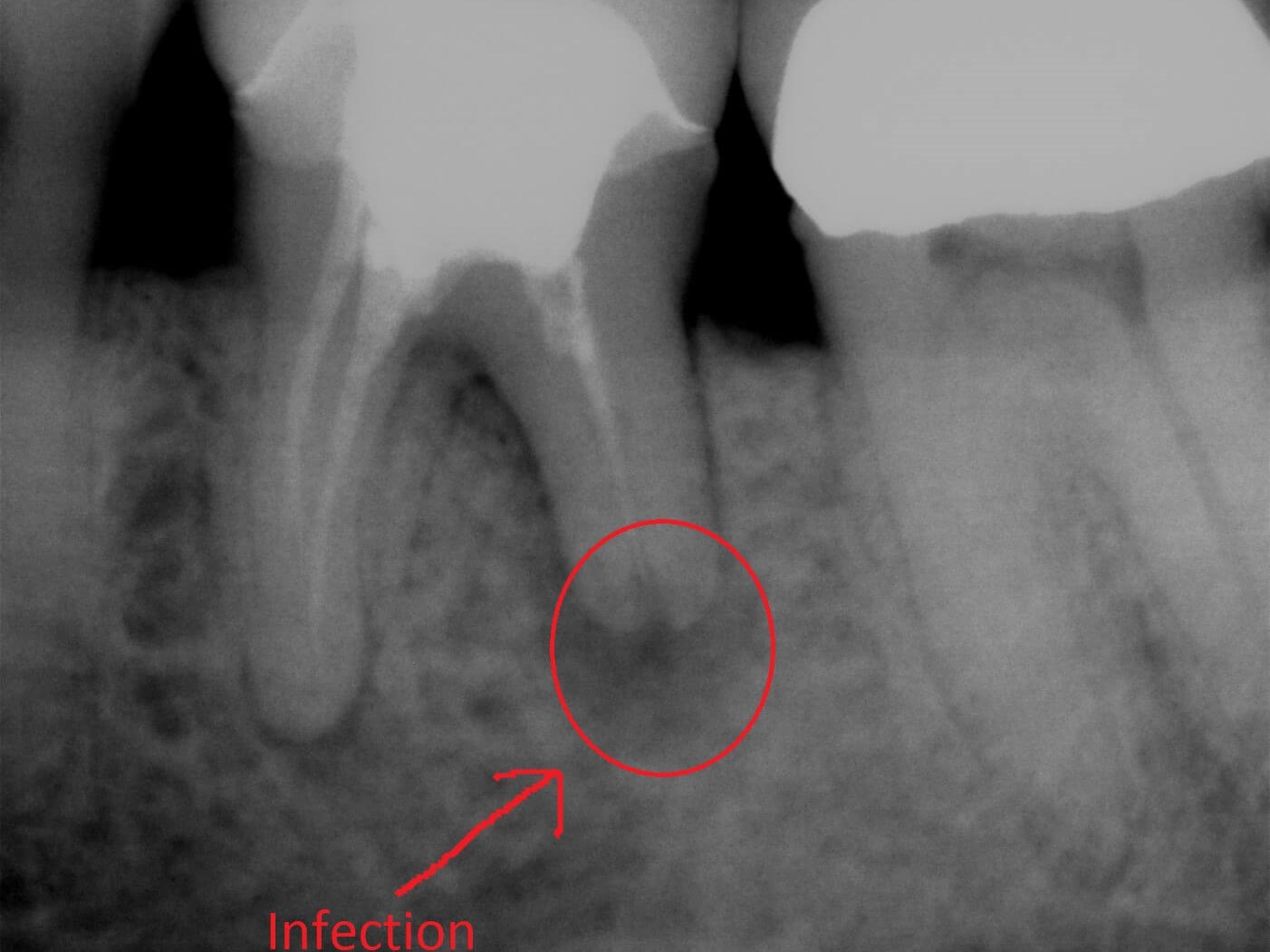
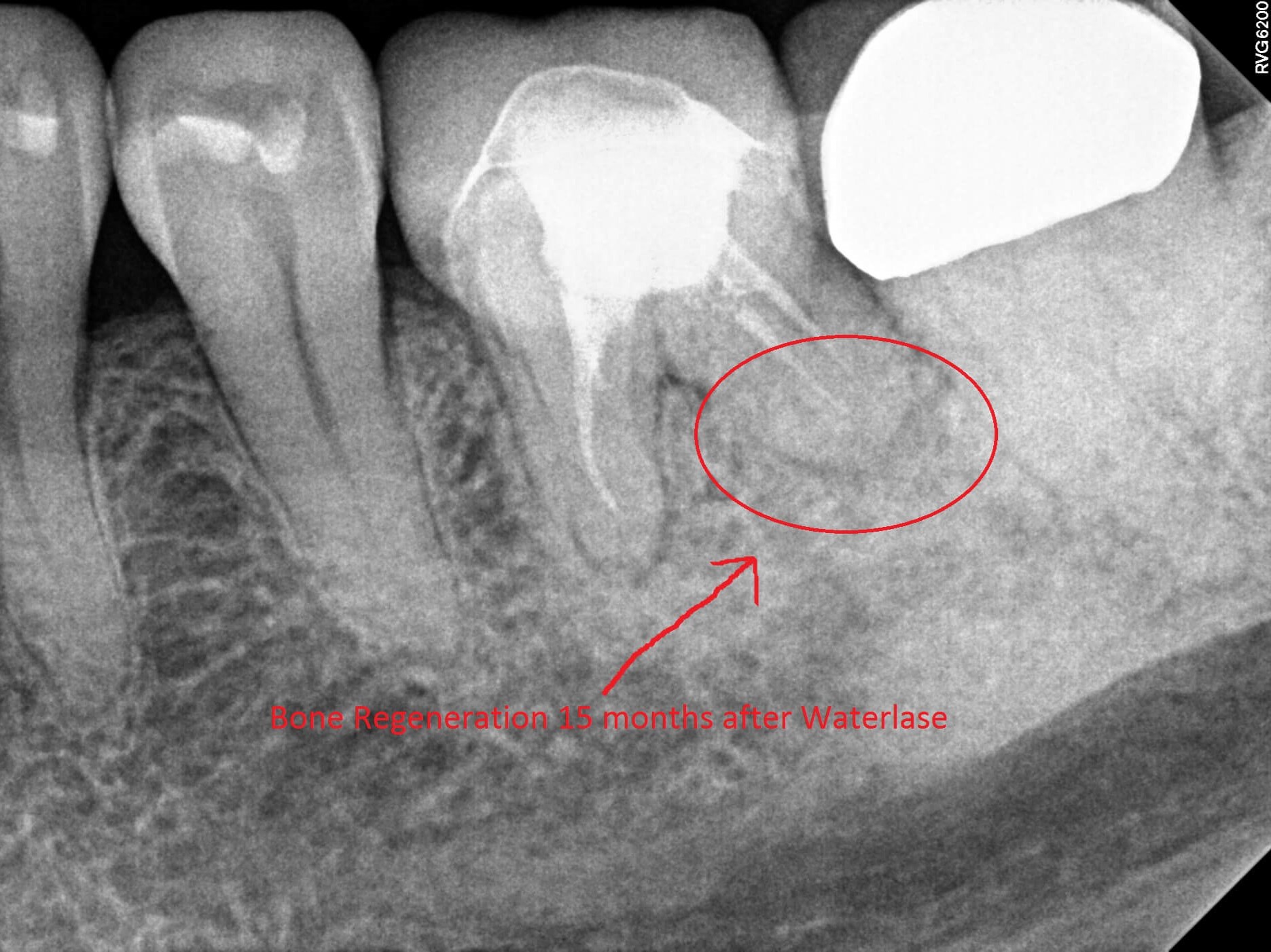
The patient presented for an emergency appointment to address pain. The tooth previously had a root canal completed, so there should not have been a feeling of pain in the actual tooth. A digital x-ray was taken and showed a PARL (Periapical Radiolucency, a change indicating bacteria and infection at the tip of the tooth root.) A periodontal (gum) and endodontic abscess was diagnosed as well as minimal bone loss. An incision and drainage along with antibiotics were recommended as treatment. Using the Waterlase laser, Dr. Patel accessed the infection, cleaned out the bacteria and diseased tissue below the gum line and around the bone. We continued to monitor the patient at follow up appointments. Another digital x-ray, shown here, was taken 15 months later and bone regeneration was noted. She was able to continue with her routine care in our office.


Procedure Details
The patient presented with concern about an old silver filling that had begun to chip away on her upper left. She was embarrassed about the look and condition of the tooth. During her exam, a digital x-ray revealed recurrent decay under the existing amalgam filling and cracks within the tooth. The old filling was removed and the tooth was excavated with the help of our WaterLase laser to access the subgingival decay. Due to the extensive decay, Dr. Patel recommended that a pulp cap be placed to help protect the unexposed nerve tissue. The tooth structure was built up for support and a crown was milled using our same day CEREC chamber. Once her occlusion was checked and any necessary adjustments were made for a correct fit and bite, the crown was permanently cemented.


Procedure Details
The patient presented with broken teeth and an esthetic concern. A digital x-ray revealed a deep depth of decay in the patient's last three lower left teeth. Intraoral photos were taken and reviewed with the patient in order for him to visually see the need for treatment. Dr. Patel recommended composite tooth colored fillings. The teeth were excavated with laser assistance to access decay below the gum line. Composite tooth-colored fillings were placed, his occlusion was checked and bite adjusted. The patient will return for his routine hygiene appointments.

Procedure Details
The patient presented for an emergency visit due to a broken tooth. During an exam with Dr. Patel, digital x-rays revealed a vertical crack, requiring a root canal. The tooth was excavated and evaluated, while an intraoral camera was used to record diagnostic photos of the treatment process. The canals were cleaned and disinfected with the help of our Biolase laser and then filled with a material called "gutta percha". Dr. Patel placed a temporary filling at the access until the patient returned a week later for her permanent crown. The temporary filling was taken out and once all decay was removed, the remaining tooth structure was insufficient to support a crown. A post was placed and the tooth was built up to provide stability. Using our CEREC computer and milling chamber, Dr. Patel designed a crown that was then cemented the same day.

